

Deep Transcranial Magnetic Stimulation, or Deep TMS™, has been shown to safely and effectively alleviate the symptoms of obsessive-compulsive disorder (OCD), particularly those patients who have not achieved sufficient improvement from traditional OCD treatment options.
The treatment utilizes a magnetic field emitted by BrainsWay’s patented H7-coil to directly reach broader and deeper brain regions than its predecessors, regulating the neural activity of brain structures associated with OCD – specifically the anterior cingulate cortex and medial prefrontal cortex.
A peer-reviewed multicenter clinical study found Deep TMS to be a highly effective OCD treatment, with more than one in three treatment-resistant OCD patients achieving “response”, greatly improving their quality of life.
As a noninvasive procedure, Deep TMS is a well-tolerated treatment that does not cause any adverse or long-lasting side effects. It does not require a significant recovery period, and the 18-min treatment can easily be integrated into each patient’s day-to-day schedule.
 Obsessive-compulsive disorder, or OCD, is a mental disorder defined as a combination of anxiety-inducing thoughts and behavior. OCD can be time-consuming, create significant distress on the individual facing it and take a toll on family, friends, and colleagues.
Obsessive-compulsive disorder, or OCD, is a mental disorder defined as a combination of anxiety-inducing thoughts and behavior. OCD can be time-consuming, create significant distress on the individual facing it and take a toll on family, friends, and colleagues.
The condition’s two main components are ruminative thoughts (“obsessions”) and the actions meant to soothe them (“compulsions”).
Obsessive Thoughts: OCD usually arises from distressing, repetitive thinking. Common categories that fuel OCD-related anxiety include:
Compulsive Behavior: When battling OCD, many patients develop compulsive, ritualistic behavior as a way to suppress their stressful thought content – for example, excessive hand washing.
 While these compulsive behaviors are meant to help reduce anxiety, in time they are incorporated into the individual’s obsessive OCD patterns, until they begin inducing stress themselves. This creates a cycle of thoughts and actions that exhaust the individual experiencing them, causing them a great deal of despair.
While these compulsive behaviors are meant to help reduce anxiety, in time they are incorporated into the individual’s obsessive OCD patterns, until they begin inducing stress themselves. This creates a cycle of thoughts and actions that exhaust the individual experiencing them, causing them a great deal of despair.
OCD Demographics: According to the DSM V, OCD occurs in 1.2% of the population. While females are found to be affected at a slightly higher rate than males, males are more likely to develop OCD during childhood.
Possible Causes for OCD: OCD has been found to be associated with a number of risk factors, such as genetics, environmental factors, temperament and critical life events. Those with OCD also often battle additional mental health conditions, with three in four having a history of anxiety disorders, and nearly one in two battling depression.
 Deep TMS: The first noninvasive device FDA-cleared to treat OCD, Deep TMS utilizes magnetic fields to safely regulate the neural activity of brain structures found to be related to OCD. A multicenter study published in 2019 by the American Journal of Psychiatry confirmed the treatment’s efficacy, concluding that focusing brain stimulation on “the medial prefrontal cortex and anterior cingulate cortex significantly improved OCD symptoms.” Deep TMS is also safe to combine with other forms of therapy, and does not cause any adverse or long-lasting side effects. It is noninvasive and can be easily incorporated into the patient’s daily schedule.
Deep TMS: The first noninvasive device FDA-cleared to treat OCD, Deep TMS utilizes magnetic fields to safely regulate the neural activity of brain structures found to be related to OCD. A multicenter study published in 2019 by the American Journal of Psychiatry confirmed the treatment’s efficacy, concluding that focusing brain stimulation on “the medial prefrontal cortex and anterior cingulate cortex significantly improved OCD symptoms.” Deep TMS is also safe to combine with other forms of therapy, and does not cause any adverse or long-lasting side effects. It is noninvasive and can be easily incorporated into the patient’s daily schedule.
Cognitive Behavioral Therapy: CBT is a form of psychotherapy commonly used to treat OCD. The treatment focuses on the thoughts, feelings, behavior and physical reactions linked to OCD, while helping patients become less anxious in reaction to them. One subtype, Acceptance and Commitment Therapy (ACT), assists patients in developing openness and flexibility when reacting to obsessive thoughts, while committing to behavioral change.
 Exposure and Response Prevention Therapy: ERP has also been shown to be a form of psychotherapy effective in treating OCD. ERP gradually exposes the patient to the source of their anxiety, accompanied by the support of a mental health professional, who encourages them to refrain from acting on their compulsions.
Exposure and Response Prevention Therapy: ERP has also been shown to be a form of psychotherapy effective in treating OCD. ERP gradually exposes the patient to the source of their anxiety, accompanied by the support of a mental health professional, who encourages them to refrain from acting on their compulsions.
Psychopharmacology: Medication for OCD is also considered among the treatment options found helpful in reducing OCD symptoms. Several antidepressants have been FDA-approved to treat OCD, including selective serotonin reuptake inhibitors (SSRIs) and one tricyclic antidepressant (TCA). While many patients find them to be helpful, these medications can also induce possible side effects, such as weight gain and sexual dysfunction.
Lifestyle Changes to Protect Against OCD: Healthy eating, regular exercise and “sleep hygiene” (eliminating distractions when going to bed) are seen as a “winning triad” that greatly affects our ability to ward off OCD symptoms. Additional protective factors include keeping up with your regularly scheduled activities and incorporating stress management techniques such as meditation, yoga, and massage therapy into your life.
BrainsWay’s Deep TMS OCD treatment using the H7-coil significantly alleviates OCD symptoms, as demonstrated in a 2019 multicenter, double-blind, randomized controlled clinical study published by the American Journal of Psychiatry.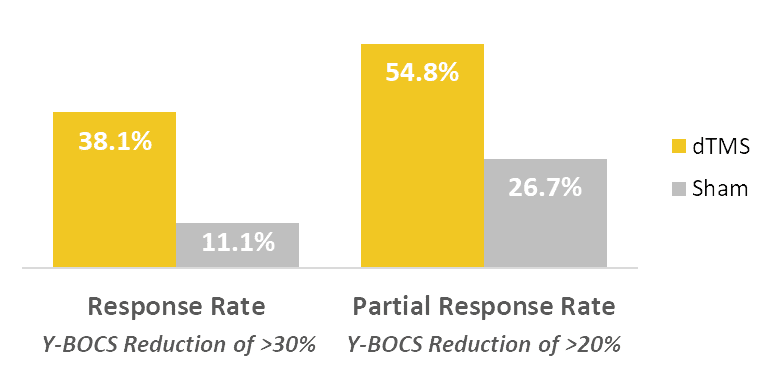
The 2019 study concluded that after six weeks of treatment, there was a statistically significant improvement in OCD symptoms for the study’s active treatment group when compared to the sham group. The study also found the improvement was maintained at least one month after the treatment’s end, at week 10.
The primary measuring system used in this study was the Yale-Brown Obsessive-Compulsive Scale (Y-BOCS), the gold standard measure of OCD symptom severity. It found that 38.1% of patients in the active group achieved a full response reduction in symptom severity, compared to just 11.1% in the sham group. Additionally, 54.8% of patients in the active group achieved a partial response of reduction in symptom severity, versus just 26.7% in the sham group.
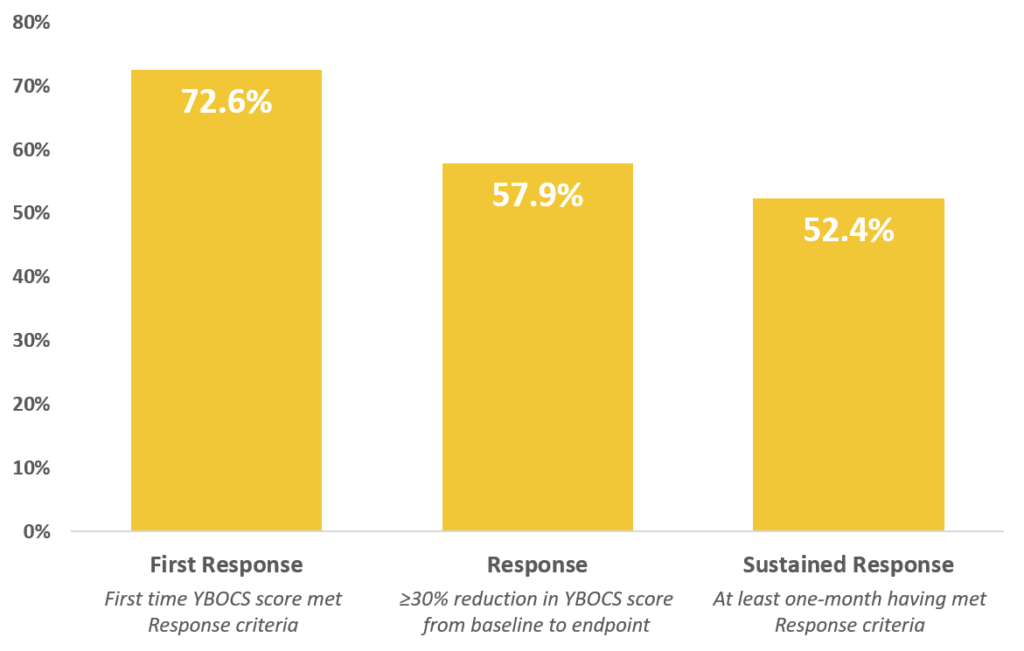
Based on a post-marketing study of over 200 patients published in the Journal of Psychiatric Research, Deep TMS has been shown to have an even greater effect in a real-life clinical practice setting. Nearly 60% of patients achieved response, defined as >30% YBOCS reduction from endpoint to baseline, after 29 sessions. >70% of patients reached first response after an average of 18.5 Deep TMS sessions or 31.6 days. >50% of patients achieved a sustained response (one-month meeting response criteria) after an average of 20 sessions or 32.1 days.
 As a noninvasive treatment course, Deep TMS does not necessitate anesthesia, does not cause any significant side effects, and can be incorporated into the patient’s schedule with ease.
As a noninvasive treatment course, Deep TMS does not necessitate anesthesia, does not cause any significant side effects, and can be incorporated into the patient’s schedule with ease.
Deep TMS has been proven to be a safe treatment option by a number of studies. A 2018 study published by Brain Stimulation Journal highlighted Deep TMS’s safety, finding it to be a safe OCD treatment: “Deep TMS stimulation over the mPFC (medial prefrontal cortex) and ACC (anterior cingulate cortex) is a safe and effective intervention for improving OCD symptoms in patients who failed to receive sufficient benefit from treatments with SRIs and CBT.”
BrainsWay’s Deep TMS technology includes a patented H-Coil, held inside a cushioned helmet that is fitted onto the patient’s head. Once activated, the H-Coil sends a magnetic pulse that acts to regulate the brain’s neural activity.
Deep TMS sessions for OCD treatment involve a brief personalized provocation, or exposure, to activate the relevant areas of the brain, followed by an 18-minute TMS treatment. A full course of BrainsWay OCD usually requires daily sessions over a six-week period.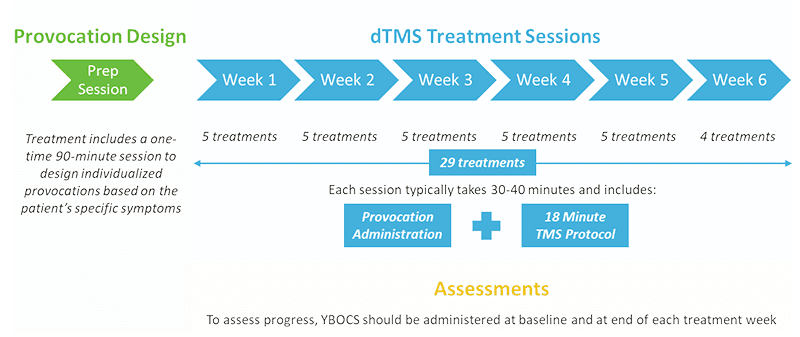
Here how an OCD patient’s quality of life significantly improved after BrainsWay OCD treatment by Dr. Ryan Vidrine of TMS Health Solutions.
Check out additional testimonials of patients and healthcare providers in our video gallery.
Publication & Date:Brain Stimulation9:1-9 (2016)
Investigators:A Zangen, L Carmi, U Alyagon, J...
Depression is a neuropsychiatric disorder that is expressed in emotional, physiological, and behavioral...
Anti-psychotic medications are often effective for the positive symptoms of schizophrenia