A growing body of research has cited high Deep TMS™ therapy success rates, finding that BrainsWay’s Deep Transcranial Magnetic Stimulation (Deep TMS) can alleviate symptoms of a number of mental health conditions. Such studies rely on meticulous, evidence-based analysis whose results have been published in prestigious medical journals.
Studies on Deep TMS leverage gold-standard benchmarks, such as double-blind, randomized control trials (RCT) and multicenter patient arms to maximize their objectivity. 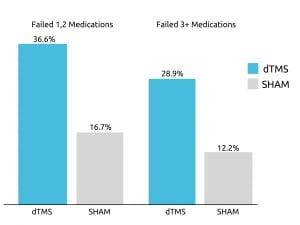 One such study from 2015, published in World Psychiatry, received data from 20 different academic mental health centers to examine Deep TMS’s effect on treatment-resistant participants battling Major Depressive Disorder (MDD).
One such study from 2015, published in World Psychiatry, received data from 20 different academic mental health centers to examine Deep TMS’s effect on treatment-resistant participants battling Major Depressive Disorder (MDD).
The multicenter pivotal RCT, which was the foundation for BrainsWay receiving FDA-clearance for MDD treatment, found that roughly one out of three participants achieved remission after four weeks of Deep TMS treatment included in the acute phase. This was true even among patients who had previously failed to sufficiently improve from three or more antidepressant medications.
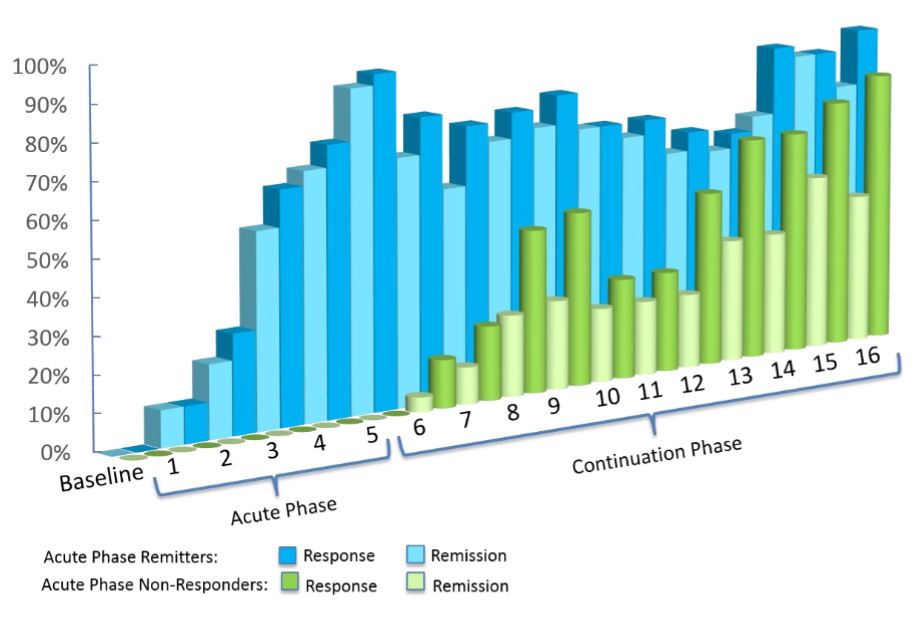
Additionally, over 80% experienced a response (or improvement) during the following continuation phase.
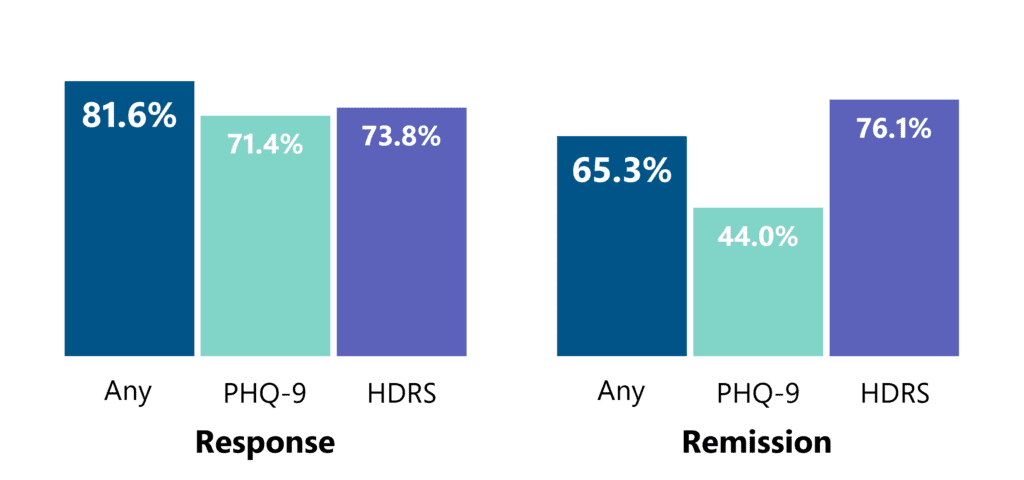
Clinical data of over 1,300 patients in real practice settings has shown compelling results. Among patients who completed at least 30 sessions, approximately 4 in 5 achieved a response and approximately 2 in 3 achieved remission.
BrainsWay Deep TMS technology has also been clinically validated to treat OCD. A study published in 2019 in the American Journal of Psychiatry found that a six-week course of BrainsWay’s Deep TMS treatment offers significant clinical improvement of OCD symptoms, with results similar to those of a 12-week pharmacotherapy treatment course. Greater than one in three patients achieved a significant reduction in OCD symptoms, including those who had previously been unresponsive to medication and/or psychotherapy. As such, Deep TMS was found to be a well-tolerated treatment that can offer about the same level of relief as medication, only in half the time.
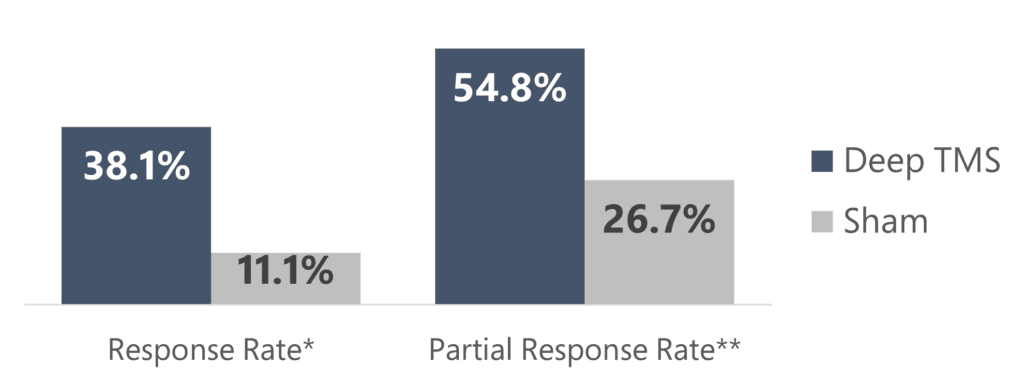
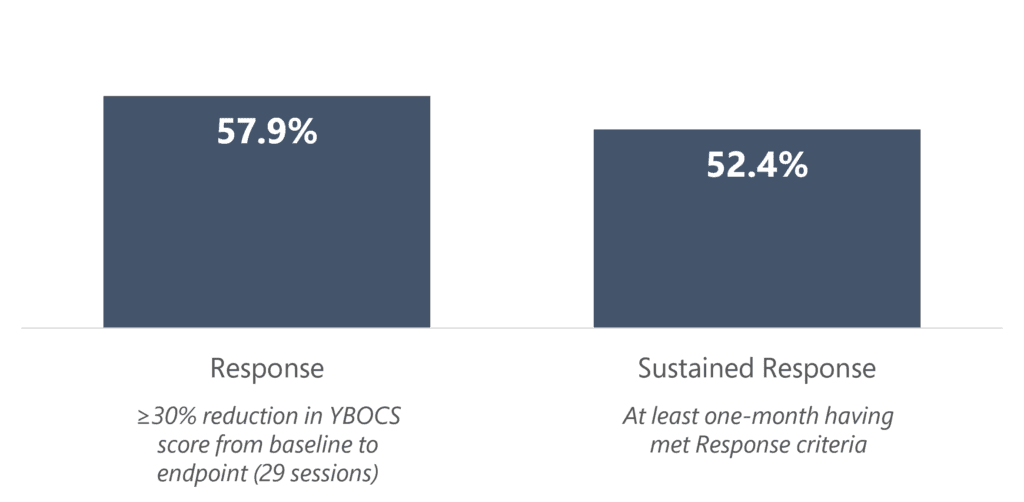
In real clinical usage of over 200 OCD patients, greater than 1 in 2 patients who received a treatment course of 29 sessions achieved response, indicating a 30+% reduction in symptoms as measured by the Y-BOCS scale.

It is safe to combine Deep TMS therapy with antidepressant medication or psychotherapy, with Deep TMS also found to offer relief when part of a combined treatment course. That said, a great deal of the research performed on Deep TMS treatment underscores its effectiveness in cases where people were found to be unresponsive to psychotherapy or SSRI medication.
In a recent study from 2019, published by the Journal of Psychiatric Research, Deep TMS therapy combined with standard medication for MDD was found to be significantly more effective than standard pharmacotherapy alone, reducing the symptoms of close to two-thirds of participants battling MDD. These results highlight Deep TMS’s ability to enhance existing treatments when administered under professional medical supervision.
Finally, a growing body of research suggests that TMS conducted during or in proximity to psychotherapy can increase the efficacy of both treatments’ combined effect.
With more and more research carried out, Deep TMS therapy’s high success rate is becoming more solidified, as the positive effects this innovative technology can have on people’s lives are becoming clearer and broader.
Read more about Deep TMS studies.