Journal: Psychiatry Research (2023)
Authors: Aron Tendler, Stephan Goerigk, Samuel Zibman, Salomé Ouaknine, Tal Harmelech, Gaby S Pell, Abraham Zangen, Steven A. Harvey, Geoffrey Grammer, Jimmy Stehberg, Oluremi Adefolarin, Owen Muir, Carlene MacMillan, Diana Ghelber, Walter Duffy, Irakli Mania, Zeeshan Faruqui, Faisal Munasifi, Todd Antin, Frank Padberg, Yiftach Roth
The safety and efficacy of the H1 Coil Deep TMS for MDD was shown in an international multicenter, randomized, controlled trial (RCT) with 212 subjects resulting in FDA clearance (Levkovitz et al., 2015), as well as in other RCTs (Filipcic et al., 2019; Matsuda et al., 2020). Deep TMS was also shown to be efficacious for depression and comorbid anxiety symptoms (Pell et al., 2022). However, the majority of RCTs do not reflect the situation of mental health care in real world settings and include only relatively small samples.
Evaluate Deep TMS for treatment of MDD in community settings, via a naturalistic study that reports the largest data set for Deep TMS and may allow new insights into Deep TMS practice and its antidepressant effects. Several objectives were pursued in analysis: (1) characterizing treatment response in a large naturalistic setting, (2) investigating the time course of clinical effects (3) investigating long-term durability, and (4) identifying predictors of response over time.
Data were aggregated from 1753 patients at 21 sites, who received Deep TMS (high frequency or iTBS) using the H1 coil. Outcome measures varied across subjects and included clinician-based scales (HDRS-21) and self-assessment questionnaires (PHQ-9, BDI-II). 1351 patients were included in the analysis, 202 received iTBS
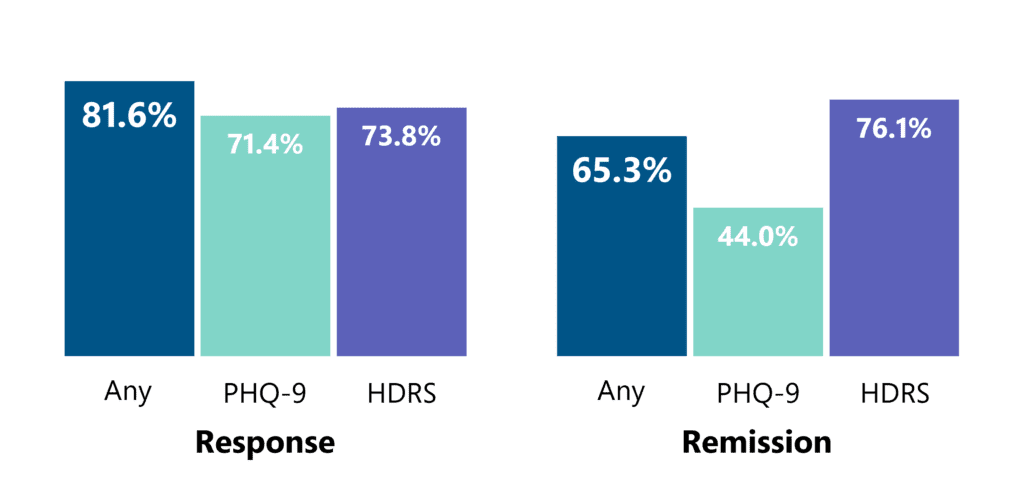
For participants with data from at least 1 scale, 30 sessions of Deep TMS led to 81.6% response and 65.3% remission rate. 20 sessions led to 73.6% response and 58.1% remission rate. iTBS led to 72.4% response and 69.2% remission. Remission rates were highest when assessed with HDRS (72%).
In 84% of responders and 80% of remitters, response and remission was sustained in the subsequent assessment. Median number of sessions (days) for onset of sustained response was 16 (21 days) and for sustained remission 17 (23 days). Higher stimulation intensity was associated with superior clinical outcomes
Beyond its proven efficacy in RCTs, Deep TMS with the H1 coil is effective for treating depression under naturalistic conditions, and the onset of improvement is usually within 20 sessions. However, initial non-responders and non-remitters benefit from extended treatment.